Hypothermia Basics for the Emergency Medicine Clinician
Introduction
As we enter winter, it becomes critically important that emergency medicine clinicians are able to rapidly recognize and respond to hypothermia. In this article, we will discuss the populations that we most commonly see hypothermia develop in, special populations, the pathophysiology of hypothermia, and the major parts of hypothermia treatment.
Incidence
As expected, hypothermia emergencies are most common in the winter months in the colder northern and Midwest states. While all populations are at risk for developing hypothermia, those with poor body fat reserves and those are under constant exposure without proper protection are at highest risk. The elderly and infants are at especially high risk due to their poor body fat reserves and inability to seek shelter in a timely manner on their own. Unhoused people are also at high risk, especially in areas without rewarming centers available. Other populations that you should have a high index of suspicion for hypothermia include outdoor workers such as linemen, sanitation workers, oil & gas workers, and fishermen. Indoor workers such as refrigeration plant and food processing workers are also at risk.
Pathophysiology
Hypothermia occurs at 35 C and below. It is important to note that these are for core body temperatures only, and that axillary or tympanic membrane assessment are not necessarily reliable means of assessing hypothermia severity.
Mild Hypothermia - 32-35 C - The first stage of hypothermia is typically well tolerated and includes nonspecific symptoms such as pale appearance, shivering, musculoskeletal pain, and poor cognition. The body begins compensating by increasing metabolism through tachycardia, tachypnea, and shivering to produce heat and increase CBT. The body additionally vasoconstricts peripheral vasculature to reduce the available vascular surface area and thus retain heat.
Note: Shivering uses the constant movement and contraction of skeletal muscles to burn fat. That means those with more muscle mass will compensate better, and those with less (like infants and the elderly) will have less ability to compensate.
Moderate Hypothermia - 28 to 32 C - Compensatory mechanisms begin to fail at this point. Hypotension can develop, and HR can drop. Altered mental status is common. Vasoconstriction begins to fail. Shivering often stops during this stage, worsening the decline into hypothermia as the body loses its ability to compensate.
Severe Hypothermia - Under 28 C - Compensatory mechanisms have failed. These patients will often be unresponsive as perfusion drops. Hypotension, bradycardia, hypoxia, and pallor are expected. Metabolism has slowed to the point that it cannot sustain life.
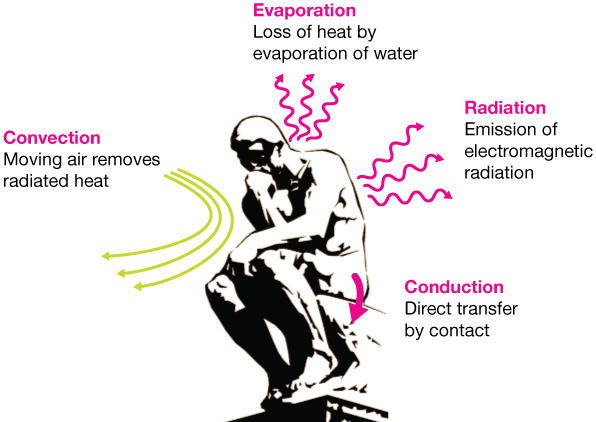
Credit eastman.com. Image above shows the four means by which we lose heat.
EKG Changes Associated with Hypothermia
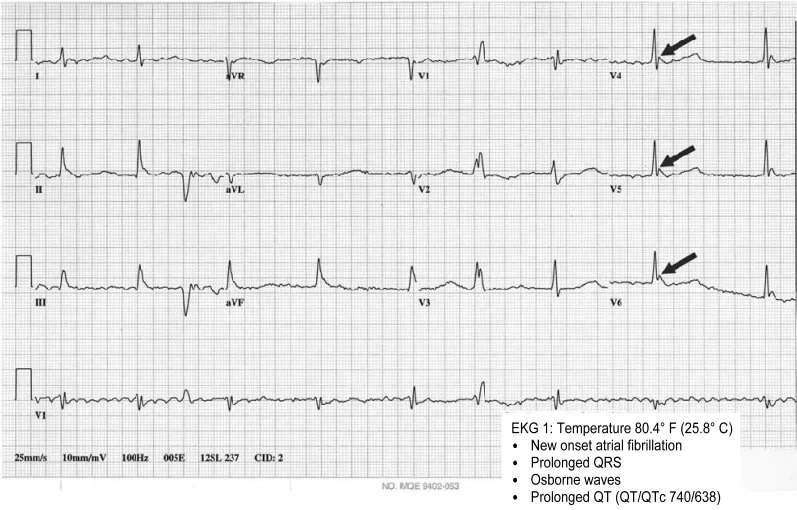
EKG changes are common with moderate to severe hypothermia and can be important assessment factors to consider. As patients become more hypothermic and their conduction overall slows, they become bradycardic. Both the QT and PR interval prolong (AHA).
Severe hypothermia (<86F/<32C) can cause a progressive widening of the QRS and risk the development of ventricular fibrillation. Take caution when moving these patients, as their already irritable hearts can be pushed into a dysrhythmia
Osborne/ J Waves
Osborne waves are a classic finding of significant hypothermia in which the J point develops a notched appearance that can resemble delta waves (Mareedu et al., 2008). These do not necessarily serve as an indicator of mortality, but they are roughly proportional to the degree of hypothermia present (Mareedu et al., 2008).
Sourced from research article. This EKG shows highlighted Osborne waves.
Assessment
Assessing the environmental conditions you find the patient in can be just as important as assessing themselves. Is it cold outside? Is there a wind chill? Does the patient have adequate protection, either by shelter or clothing, from the elements? How long have they been exposed to the elements? Is their clothing wet or otherwise compromised? Is their heat working in the home? Maintain a high index of suspicion for hypothermia in any patient that has had prolonged time spent outdoors.
Classic populations to look for hypothermia in include the unhoused, those consuming alcohol outdoors, and blue-collar workers.
You should also try to identify if the cause of the hypothermia is environmental or not. Many things can cause hypothermia, including trauma/shock, sepsis, substance use/toxicity, and adrenal conditions. While all hypothermia must be corrected, your history taking and assessment should be steered by the suspected underlying cause.
Core body temperature is the only reliable way to assess hypothermia. It is often difficult in the prehospital realm. Oral temperatures fail at lower temperatures. CBT such as esophageal probes, rectal probes, catheter probes are the gold standard.
Treatment
The general cornerstones of hypothermia management include removal from the cold environment, active rewarming, supporting vital needs such as oxygenation and blood pressure, and treating secondary complaints such as pain. Remove wet or cold clothing and replace with dry. Remove constricting items as they may worsen tissue ischemia in extremities.
Avoid secondary instances of hypothermia. It may be best to delay active rewarming efforts if you are still in the cold environment until you are able to ensure they will not become hypothermic again.
Photo of a Bair Hugger; commonly used for active external warming in EDs and ICUs.
Frostbite
Frostbite is localized areas of tissue damage or death because of cold exposure. Ice crystals form within the tissues, causing ischemia. It is most commonly found in the digits such as the toes and the fingers but can affect anywhere.
Rewarm the affected digit with warm water (ideally 104F) immersion and avoid drying or aggressive manipulation, as this can cause further damage. Wrap with warm linens once rewarming is done, and protect from further hypothermia/exposure (Wagner, 2023).
Severe enough frostbite can constitute burn center referral. It may be of use to consult with a tertiary, burn capable center when treating patients with significant frostbite (Wagner, 2023).
Frostbite is extremely painful; treat for pain appropriately using your available medications.
Mild Hypothermia
Mild hypothermia will typically resolve with removal from the cold environment and simple blankets/dressing. Mild cases will not require further management.
Moderate Hypothermia
Moderate hypothermia will require removal from the cold environment and active rewarming. Apply copious blankets, increase ambulance HVAC to hot (you should be sweating!) and provide warmed fluids if available.
You may use heat packs between blanket layers prehospital to provide additional warming. Avoid skin burns from direct contact.
Correct apparent hypovolemia with fluids if necessary; however, these patients often do not require significant fluid boluses.
Bradycardia is often present but does not require acute treatment if hemodynamically stable. Focus on rewarming and not necessarily rate adjustment; you can risk ventricular dysrhythmias due to the heart’s inherent, already-present irritability with hypothermia.
Atropine and sympathomimetics are not usually indicated. Correcting the underlying hypothermia will usually reverse the bradycardia and hypotension.
Severe Hypothermia
Severe hypothermia requires active rewarming, including the use of heat packs, HVAC heat, blankets, and warmed fluids if available.
Exercise extreme caution when moving these patients.
Severely hypothermic patients are prone to ventricular dysrhythmias
In-hospital, the patient may receive gastric/bladder/chest tube lavage with warm fluid to allow for active core rewarming.
Special Cases & Miscellaneous Information
Submersion Injury/Drowning with Hypothermia
Submersion injuries with hypothermia onset are delineated by if they became hypothermic prior to submersing or they submersed and then became hypothermic (Singh, 2015). There is often no reliable way to know beyond good history taking and environmental assessment, but we regardless must focus on both correcting the underlying hypoxia through advanced airway management in addition to rewarming efforts. These patients should not be terminated in the field and must ideally be transported to an ECMO/ECLS capable center, as their complex pathology may benefit from ECMO placement (Singh, 2015).
Hypothermic Cardiac Arrest
As we discussed above, hypothermia ultimately kills by slowing metabolism until it becomes insufficient to sustain life. Drugs metabolism becomes less effective. Hypothermic cardiac arrest management focuses on staged rewarming in addition to usual ACLS. While exact protocols vary by area, we will use the European Resuscitation Council Guidelines of 2021 as an example of the differences that can be present with hypothermic cardiac arrest (Soar et al., 2021).
<28C: Medications assumed to not metabolize because of inadequate circulation. Attempt defibrillation but withhold if no success in conversion after 3x defibs until 30C achieved.
>30C: Metabolism is assumed to be slow. Increase time between administrations.
Resuscitation cannot be terminated until a minimum of 32C CBT, and patients should never be terminated prehospital with limited exceptions.
Examples of exceptions include chest wall and airway freezing preventing compression, total freezing without ability to extricate the patient, avalanche with airway collapse over a prolonged period, and other obvious findings incompatible with life such as decapitation.
Afterdrop Phenomenon
Caution should be exercised with any rewarming, especially with significantly hypothermic patients. As the extremities warm and begin vasodilating during rewarming, it causes acidotic and still-cold blood to return to central circulation. This undoes any compensation that the core essential organs have been doing and can cause rebound hypothermia, hyperkalemia (from ischemic tissues dumping potassium during rhabdomyolysis -> releasing potassium), and acidosis (the blood in the periphery is going to be ischemic and thus acidotic during prolonged hypothermia). Expect some drop in blood pressure as rewarming occurs because of the reduction in vasoconstriction (Ahsan, n.d.).
Controlled rewarming and preventing a second episode of hypothermia is critically important. Active rewarming in the prehospital world should be attempted but may not be as effective as core warming done in the hospital. Regularly reassess your progress while rewarming to ensure that you are not risking afterdrop.
Cold Diuresis
Fluid loss can occur due to “cold diuresis” resulting from hypothermia (Duong & Patel, 2024). These patients may have adequate urine output but still hypoperfused from hypovolemia due to fluid loss. Replenish fluids as needed especially with prolonged care.
Summary
Correcting hypothermia requires a careful yet aggressive balance of fluid resuscitation, active rewarming, and general supportive care witth critical patients. Core body temperature monitoring should care your resuscitation; however, it is important to remember the inherent limitations of any CBT monitoring in prehospital 911 services without invasive monitoring ability. Consider transporting to ECMO/ECLS capable hospitals when feasible and remember that these patients are a must-transport in almost all scenarios (despite of the growing trend towards TOR at the scene).
References
Ahsan, S. (n.d.). Hypothermia. Core EM. https://coreem.net/core/hypothermia/
Alhaddad, I. A., Khalil, M., & Brown, E. J. (2000). Osborn Waves of hypothermia. Circulation, 101(25). https://doi.org/10.1161/01.cir.101.25.e233
Duong, H., & Patel, G. (2024, January 19). Hypothermia. StatPearls - NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK545239/
Mareedu, R. K., Grandhe, N. P., Gangineni, S., & Quinn, D. L. (2008). Classic EKG changes of hypothermia. Clinical Medicine & Research, 6(3–4), 107–108. https://doi.org/10.3121/cmr.2008.809
Singh, M. (2015, April 6). Hypothermia and Drowning Pearls - EMDocs. emDocs. https://www.emdocs.net/hypothermia-and-drowning-pearls/
Soar, J., Böttiger, B. W., Carli, P., Couper, K., Deakin, C. D., Djärv, T., Lott, C., Olasveengen, T., Paal, P., Pellis, T., Perkins, G. D., Sandroni, C., & Nolan, J. P. (2021). European Resuscitation Council Guidelines 2021: Adult advanced life support. Resuscitation, 161, 115–151. https://doi.org/10.1016/j.resuscitation.2021.02.010
Wagner, A. (2023). Frostbite Management Guidelines. https://www.vumc.org/burn/sites/default/files/public_files/Protocols/Frostbite%20Management%20-%20January%202023.pdf